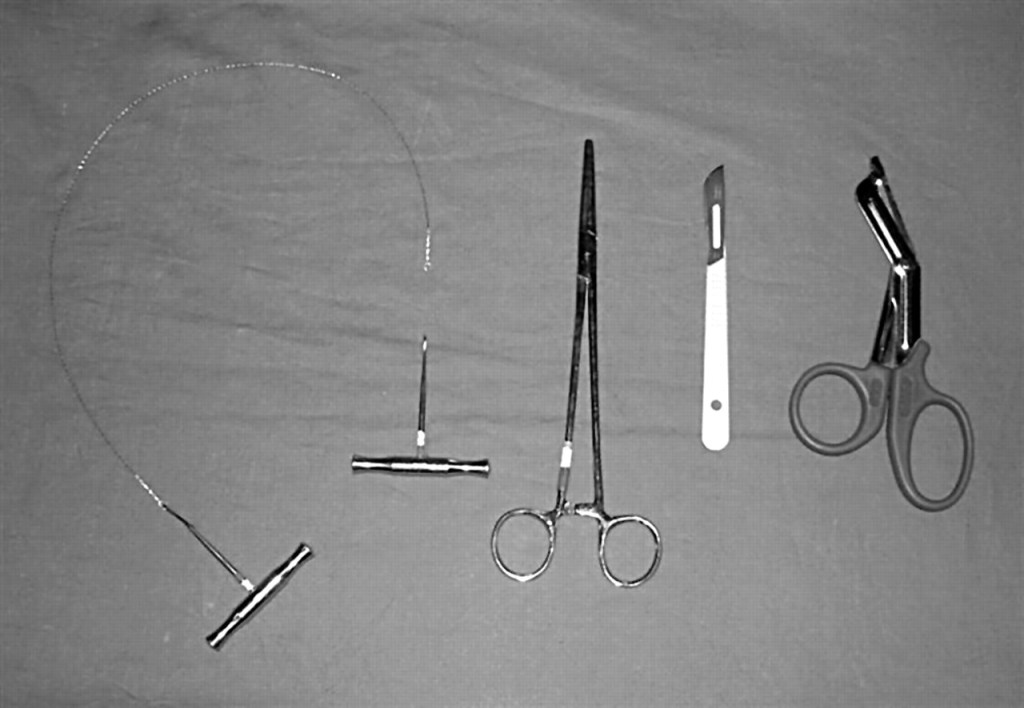
Tools required for resuscitative thoracotomy (left to right): Gigli saw (if required), Spencer-Wells artery forceps of appropriate size, scalpel and tough cut scissors.
About the podcast
Matt Warner is a consultant in Emergency Medicine and Prehospital Emergency Medicine and the Major Trauma lead for the Peninsula MTC, Derriford Hospital in Plymouth. Having experience of prehospital care in several different systems within ther UK and overseas, we’ve asked Matt to share his expert knowledge of the topic of traumatic cardiac arrest.
Traumatic cardiac arrest is the result of cardiovascular collapse either from obstructive shock (in the case of tension pneumothorax and cardiac tamponade) or haemorrhagic shock from exsanguination. Matt highlights how the resuscitative thoracotomy needs to be viewed in the same light as our other haemorrhage control measures (i.e. pelvic and long bone splinting, rapid transfusion etc.) and not simply the default action in traumatic cardiac arrest. He also discusses some of the cognitive stop points useful in this situation.
Moving onto the procedure of the thoracotomy, Matt and Tim discuss the HOT principle to guide both decision to perform and actions taken during the thoracotomy. There will be an accompanying video for the procedure of the resuscitative thoracotomy coming soon so keep an eye on the videocasts.
Check the show notes for the learning areas for the level 1 and 2 Major Trauma Nursing competencies covered in this podcast, along with other useful resources and recommended podcasts.

Traumatic Cardiac Arrest – ThePTN podcast
Learning areas in this podcast:
- Understands that needle decompression is not the recommended 1st line treatment of tension pneumothorax in hospital (NICE 2016) but that patients may present with needle decompression device(s) in-situ from the prehospital setting
- Can describe the procedure for an emergency thoracostomy including relevant anatomy and physiology. Is able anticipate the need for an emergency thoracostomy(s) and is able to lead in the preparation of an emergency thoracostomy
- Can describe the procedure for chest drain insertion including relevant anatomy and physiology. Is able anticipate the need for and lead in the preparation for a chest drain and assist with chest drain insertion
- Can describe the indications and contra-indications for a thoracotomy including relevant anatomy and physiology. Is able anticipate the need for a potential thoracotomy
Links:
Peninsula Trauma Network (PTN) Major Trauma Network guidance, Standard Operating Procedures (SOPs) here.
PTN Massive Haemorrhage SOP download here (via PTN website).
PTN Penetrating Chest Wall Injury Traumatic Cardiac Arrest and Resuscitative Thoracotomy Policy here.
RCEM Learning Emergency Department Thoracotomy here.
RCEM Traumatic Cardiac Arrest guideline located on RCEM Guideline page here.